
Date: 2025-04-04 Page is: DBtxt003.php txt00021425
US HEALTH
COVID-19
Anger over mask mandates, other covid rules, spurs states to curb power of public health officials
COVID-19
Anger over mask mandates, other covid rules, spurs states to curb power of public health officials
Original article: https://www.washingtonpost.com/health/2021/12/25/covid-public-health-laws-restricted
Burgess COMMENTARY
Peter Burgess
A new Indiana law gives city councils and county commissions power to overrule local health officials if their efforts to tame the pandemic are more stringent than rules in effect statewide. Tennessee lawmakers have taken away health officials’ ability to decide whether public schools should be closed in an emergency, giving that authority to school boards while also allowing the governor to order all schools to teach students in person.
And in Arkansas, a statute forbids any state or local official from compelling masks. As the delta variant was racing around in August, the state’s Republican governor, Asa Hutchinson, said he regretted the measure and summoned legislators into a special session to rethink it. The law stayed in place.
Conservatives frame this wave of legislating as a matter of individual liberties. Ohio state Sen. Terry Johnson (R), one of the main sponsors of that state’s new law, said last spring that its purpose is “restoring reasonable checks and balances” and “giving the people of Ohio a voice in matters of public health.”
Over the decades, critics have sought to persuade lawmakers to soften or remove safety measures, such as tobacco regulations, or requirements to wear seat belts or motorcycle helmets.
“But for them to go after the basis of public health authority is pretty new,” said Georges C. Benjamin, executive director of the American Public Health Association.
Health officials say the new laws, targeted at coronavirus-fighting strategies, often carry unintended consequences stretching far beyond the pandemic to thwart health departments'’ longtime roles, such as maintaining food safety.
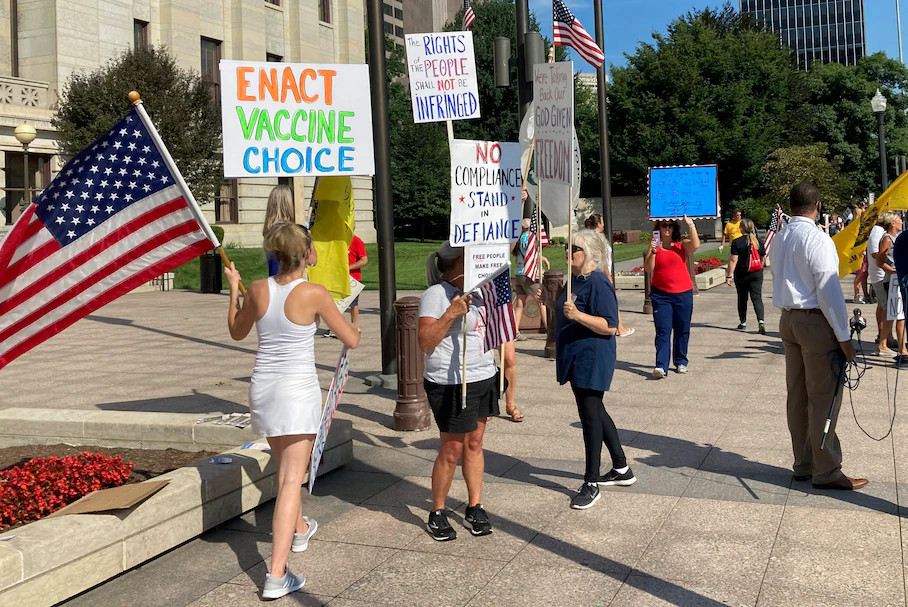
Supporters of legislation to prohibit public and private employers from requiring vaccinations or punishing workers who don't receive them rally outside the Ohio Statehouse in Columbus in August 2021. (Andrew Welsh-Huggins/AP)
The Ohio law, Senate Bill 22, slows health department’s ability to shut down a restaurant to protect customers from a foodborne disease outbreak, several health commissioners there said. Officials now can issue an order only after a person who ate there gets a documented diagnosis of such an illness — not simply after health inspectors discover unsanitary conditions.
Researchers and health officials also predict such laws will get in the way of dealing with future health crises of unforeseen origin. But as the coronavirus pandemic persists, with omicron having arrived as the most transmissible variant so far, the laws’ impact already is clear.
In May, Montana, which has several new statutes narrowing health officials’ powers, became the first state to prohibit discrimination based on vaccination status. It applies to any vaccine, not just shots to protect against the coronavirus. It means that employers may ask staff members whether they have been immunized against the virus, but they cannot punish or lay off employees who refuse to disclose their vaccination status or to get the shots. It makes an exception for nursing homes — but not for hospitals or clinics.
When the law took effect May 7, most Montana hospitals were watching the pace of the vaccine rollout and debating whether they needed to make shots essential for their workers. But just east of the Rocky Mountains, Benefis Health System, with two hospitals in Great Falls, had sent a companywide email in April announcing that, unless they had a medical or religious reason, all employees had to receive at least one shot by May 1.
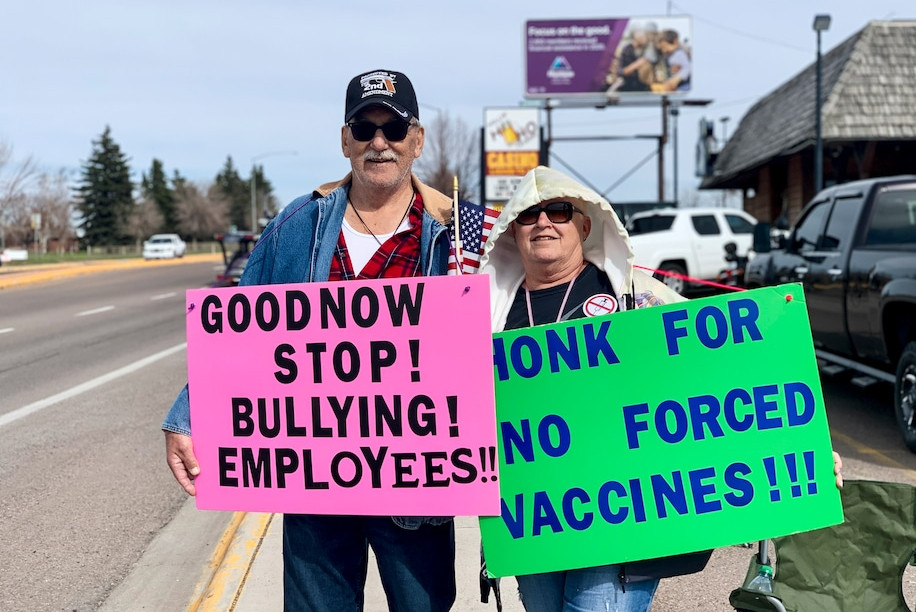
Community members staged protests. With the law imminent, Benefis backed off its mandate, according to health-care experts in the state. Benefis declined to comment on its decision.
For all 62 hospitals in the state, the law creates a bind, according to Rich Rasmussen, president of the Montana Hospital Association.
The state’s restrictions collide with what the federal government is ordering hospitals to do. The Department of Health and Human Services created a rule that hospitals and other health facilities with patients insured through Medicare or Medicaid must require their employees to have had at least a first coronavirus shot by Dec. 5.
“Hospitals were moving forward with their compliance” with the federal rule, Rasmussen said, because they feared jeopardizing $2.1 billion that flows into the state in Medicare and Medicaid payments, and most hospitals “felt a federal requirement trumped state law.”
A standoff has been averted for now, because two federal courts in November temporarily blocked the HHS requirement as part of lawsuits objecting to the federal rule. Meanwhile, a health system, a few doctors’ practices, several patients and the Montana Medical Association have filed their own lawsuit trying to restore the ability of hospitals and other health providers to compel workers to be vaccinated.
Montana’s hospitals argue they must be able to provide safe environments for their workers and patients.
“If you are providing care to neonates, you want to ensure everyone … is vaccinated,” Rasmussen said.
Many Montana employers hold a different view.
Nick Checota, a restaurant owner and music promoter who runs KettleHouse Amphitheater, a 4,500-seat outdoor venue on a river bank near Missoula, said his concert policy is to encourage patrons to wear masks and to get vaccinated or tested before attending an event. It is not required. A few bands have canceled because of the lack of vaccine verification, Checota said.
But he said, “If I’d asked my staff [to be vaccinated], half my employees would have quit. … Individual rights in Montana are very important to people.”
The political moves against vaccine requirements are spreading. Tennessee Gov. Bill Lee (R) in November signed a law that forbids employers from requiring workers, job applicants or customers to prove they have been vaccinated. Six days later, Florida Gov. Ron DeSantis (R) signed four bills that prohibit employers and educational institutions from requiring workers or students to be vaccinated against the coronavirus and removes the state health officer’s ability to order vaccinations in a public health emergency.
In Ohio, House Republicans last month passed a bill that would block employers, schools and colleges from requiring workers and students to get vaccinated if they object for “reasons of personal conscience.” Some Republicans in the state Senate are reticent, contending that businesses should be allowed to decide on vaccine policies for themselves.
Senate Bill 22, the Buckeye State’s law in effect since June, splintered the party, pitting lawmakers against Ohio’s GOP governor Mike DeWine. A year ago, DeWine vetoed another bill that would have limited the state’s coronavirus-fighting powers by handing lawmakers power to stop a governor’s public health order and tightly limiting the state health department’s ability to impose quarantines.
The bill contains those features and added restrictions on local health departments. In March, DeWine vetoed that bill, too, saying it “strikes at the heart of local health departments’ ability to move quickly to protect the public from the most serious emergencies Ohio could face.”
This time, the legislature overrode the governor’s veto on S.B. 22 the following day.
Since the law took effect, health commissioners around the state said they often have felt thwarted.

A mall sign warns shoppers to wear a mask on Black Friday in Columbus, Ohio. (Matthew Hatcher/Getty Images)
In Franklin County, which includes Hilliard, the local board of health dates to 1919, the time of a global flu pandemic that killed millions. In July 2020, as the coronavirus spread, the board ordered people to wear masks indoors, except at home. It lifted the rule the following May, weeks before the state law took effect and shortly after the Centers for Disease Control and Prevention had said people who were fully vaccinated no longer needed to wear a mask.
By late summer, cases were surging again.
“We wanted to be able to put a masking requirement in place for our jurisdictions,” said Mazzola, the Franklin County health commissioner, who works for the board.
Under the new law, only local governments can make that decision. The Franklin health district covers 14 cities, 17 townships and 10 villages. “We called on our city managers, city councils, mayors,” Mazzola said. Two of the cities, Bexley and Whitehall, reinstated mask rules. The others did not. The villages and most of the townships do not have authority to create such rules. Four townships do; they did not require masks.
“That’s really an unfortunate outcome here,” Mazzola said. “It creates mixed messaging.”
The new law also means the Franklin County health department no longer can create uniform rules for all school systems within its area.
Student vaccine mandates across California raise concerns over equity and removal from the classroom
Some school districts in California have student vaccine mandate deadlines fast approaching, raising concerns over students being removed from campus. (James Cornsilk/The Washington Post)
When the school year opened, after a year of classes mostly online, 5 of the 17 districts required masks for students and teachers in every grade, according to Ayaz Hyder, a researcher in Ohio State University’s College of Public Health who has been tracking the pandemic in nearby public schools. The first weeks of the year, the districts with universal masking had on average significantly fewer cases of the coronavirus than the rest, Hyder found.
At Hale’s Ales & Kitchen, just over the Hilliard line where there is no mask requirement, patrons are asked to wear a face covering voluntarily if they haven’t been vaccinated, workers there said. Chris Hale, the owner, did not return phone calls seeking comment.
Even when Ohio’s elected municipal officials have stepped in to adopt public health strategies of their own, controversies sometimes have swirled.
In August, the village of Gambier, home to Kenyon College, approved a temporary mask requirement for public buildings, including schools, with a $25 fine for violators. The county sheriff posted on his Facebook page that he had spoken with the mayor “and informed him that deputies will not be citing anyone for violations.”
Sheriff David Shaffer’s Facebook announcement drew more than 700 replies, mirroring the fevered views that divide the nation over public health during the pandemic.
“So … you are elected to decide which law to enforce?” one woman wrote.
Many praised the sheriff. “The more you protect our God-given freedoms,” one man wrote, “the greater my respect for you. … Please continue to defy tyrants who are trying to destroy our freedom.”
Such sentiment — and the Ohio law it yielded — leave the state’s health officials feeling impotent as each pandemic wave arrives.
In September, Jack Pepper, administrator of the Athens City-County Health Department, worried as his southeastern Ohio jurisdiction, which contains both historical Ohio University and rural poverty, suffered the largest surge in coronavirus hospitalizations and deaths of the pandemic so far.
“It would have been nice,” Pepper said, if the department could have limited the number of patrons in restaurants, as it had when establishments reopened after a pandemic shutdown early on. “Those powers are all gone.”
“In a perfect world,” Pepper said, “we would be able to do what we think is best, but that’s not our reality. So we deal with the hand we’ve been dealt.”
By Amy Goldstein Amy Goldstein is The Washington Post’s national health-care policy writer. During her three decades at The Post, her stories have taken her from homeless shelters to Air Force One, often focused on the intersection of politics and public policy. She is the author of 'Janesville: An American Story.'
----------------------------------------------------------
FROM THE WP
Coronavirus: What you need to read
Coronavirus maps: Cases and deaths in the U.S. | Cases and deaths worldwide
Vaccines: Tracker by state | Booster shots | For kids 5 to 11 | Guidance for vaccinated people | How long does immunity last? | County-level vaccine data
What you need to know: Omicron variant | Masks FAQ | Delta variant | Other variants | Symptoms guide | Follow all of our coverage and sign up for our free newsletter
MORE FROM THE POST